Telemedicine Bill in Pennsylvania May Not Pass Because Someone Mentioned the Abortion Pill

Graphic via Shutterstock / Courier
By Jen Colletta
Courier Newsroom
February 20th, 2020
The legislation would set licensing guidelines and require insurers to provide coverage for telehealth as they would in-person health care. A Republican-sponsored amendment, however, threatens to derail its passage.
Coming out as transgender in traditionally conservative rural Pennsylvania can be a frightening prospect for a teen One immediate concern they may have is whether their healthcare provider and medical staff will be affirming of their gender identity when they seek care, such as the process for blocking puberty. To complicate matters even further, the nearest pediatric endocrinologist may be a three-hour drive from home. Even if the teen has the support of parents, the distance can mean a full day of work or school missed, as well as hefty gas and toll costs.
Any rural population can face similar obstacles to obtaining care—seniors whose transport services may only cover a certain geographic area, pregnant women facing complications, patients with limited funds for travel. High-quality healthcare services, particularly specialty programs, are often anchored in urban areas.
According to the Centers for Disease Control and Prevention, Americans who live in rural areas are at a higher risk than urban residents for the five leading causes of death. It’s an issue that could hit home for many Pennsylvanians: The U.S. Census Bureau designates 48 Pennsylvania counties as rural, and, as of 2018, they were collectively home to 3.4 million people, or more than one-quarter of the state’s population.
To alleviate the disparities faced by these communities, some providers are turning to telehealth. Also known as telemedicine, the term connotes the delivery of healthcare services remotely, most commonly through videoconferencing. The practice is used for everything from routine follow-up appointments to emergency care.
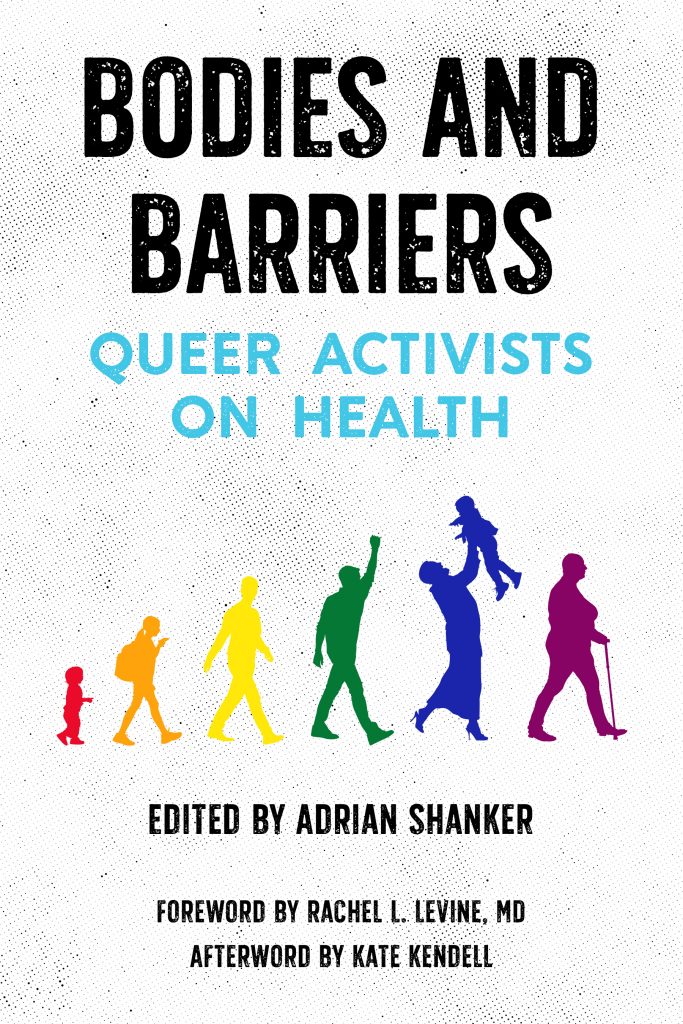
“Telehealth removes the issue of distance,” said Adrian Shanker, founder and executive director of the Bradbury-Sullivan LGBT Community Center in Allentown and author of Bodies and Barriers: Queer Activists on Health. “It makes it more possible for people in rural areas or smaller cities—especially those in multiple marginalized communities—to get quality care faster.”
Telehealth “can really help people in remote areas,” added Dr. Larry John, president of the Pennsylvania Medical Society. “I think insurers also see the value and are pushing for providers to make this available and easier on patients to get the care they need.”
John said the number of providers offering telehealth options has exploded in recent years—and he only sees that trend continuing. But, with that rapid growth, comes the need for regulations, he added.
“Right now, there are probably hundreds of providers across the country [offering telehealth] and we don’t always know their credentials, their backgrounds, where they’re licensed,” he said.
More than 40 jurisdictions in the country have laws on the books regulating telehealth. In Pennsylvania, one proposed measure has gained some traction. Sen. Elder Vogel’s (R-47) Telemedicine Act, which was first introduced in September, would set licensing guidelines and require insurers to provide coverage for telehealth as they would in-person health care. It would also allow insurance companies and providers to negotiate telehealth coverage rates—as opposed to mandating parity with rates for in-person visits.
“Some states have language saying [telehealth rates are] negotiated; others have been more prescriptive,” said Mei Kwong, executive director of the Center for Connected Health Policy and project director for the National Telehealth Policy Resource Center. “I wouldn’t say there’s one train ahead of the other.”
“Telehealth removes the issue of distance. It makes it more possible for people in rural areas or smaller cities—especially those in multiple marginalized communities—to get quality care faster.”
What is unique about Pennsylvania’s measure, however, is that a debate about abortion rights is now threatening its passage.
The state Senate nearly unanimously approved Vogel’s bill in October, but the House Insurance Committee advanced it with an amendment to prevent providers from using telemedicine to prescribe drugs on the Food and Drug Administration’s Risk Evaluation and Mitigation Strategies (REMS) list, a database of potentially risky medications. Among the drugs on that list is an abortion-inducing pill regimen called mifeprex, which can end a pregnancy up to 70 days.
Vogel’s bill was almost successful in late 2018, but Rep. Kathy Rapp (R-65), the chair of the Pro-Life Caucus, introduced a similar REMS amendment that halted the voting process.
This time around, the House adopted the bill nearly along party lines in November and it now heads back to the Senate for its approval on the new language; a vote in the Senate has not yet been scheduled.
While the bill initially had broad bipartisan support, that appears to have been eroded.
“Our caucus is for the version that left the Senate,” Brittany Crampsie, press secretary for the Senate Democratic Leader and Caucus, told COURIER. “The House amendment is anti-choice and limits access to a whole list of other pharmaceutical products.”
A spokesperson for Gov. Tom Wolf didn’t respond to a request for comment, but has said publicly the governor no longer supports the legislation.
Kwong noted that while other jurisdictions have debated the REMS issue in regard to telehealth, that question isn’t usually attached to an insurance-focused bill like Pennsylvania’s proposed measure.
“This is a more unusual vehicle for that [anti-abortion amendment],” she said. “If states are going to pass a statute limiting the use of telehealth in prescribing an abortion drug, it’s typically been done around a prescribing law that focuses on how to use telehealth, as opposed to this type of law.”
Healthcare decisions, Shanker said, should be made solely between a patient a provider, “and not by what a politician thinks might help them in terms of their public support. That’s not what the purpose of medicine is. Telehealth should be available as a tool to help people access care, not limit it.”abortionhealthpennsylvaniatelehealthtelemedicine
Jen Colletta is a Philadelphia native currently working as a writer and editor in the B2B publishing world. She is the former editor of Philadelphia Gay News, where she picked up more than 50 state and national writing awards.